There’s only thing more confusing and stressful than figuring out life after blood clots.
Navigating menopause and aging well as a woman who has survived blood clots.
The National Institute on Aging estimates that 1 million women go through menopause each year in the United States.
That number doesn’t include younger women who have gone through surgical menopause.
Recent studies asking peri and post-menopausal women how much they knew about menopause revealed a gap in both knowledge and reliable education.
In women under 40, an online study analyzed 738 women’s responses and 80% had no knowledge or just some knowledge of menopause.
PMID: 36533635
A similar study analyzed data from 829 women who identified as postmenopausal:
49.0% did not feel informed at all about menopause. More than 60% started looking for information regarding menopause as their symptoms started.
PMID: 36994487
According to those online studies, there were six themes identified when it comes to the menopause information gap:
- The need for education.
- Knowledge and understanding of menopause symptoms.
- Why is getting treatment so difficult?
- Feelings and attitudes towards menopause.
- The impact of menopause on a woman’s life.
- The importance of the media – are they getting it right?
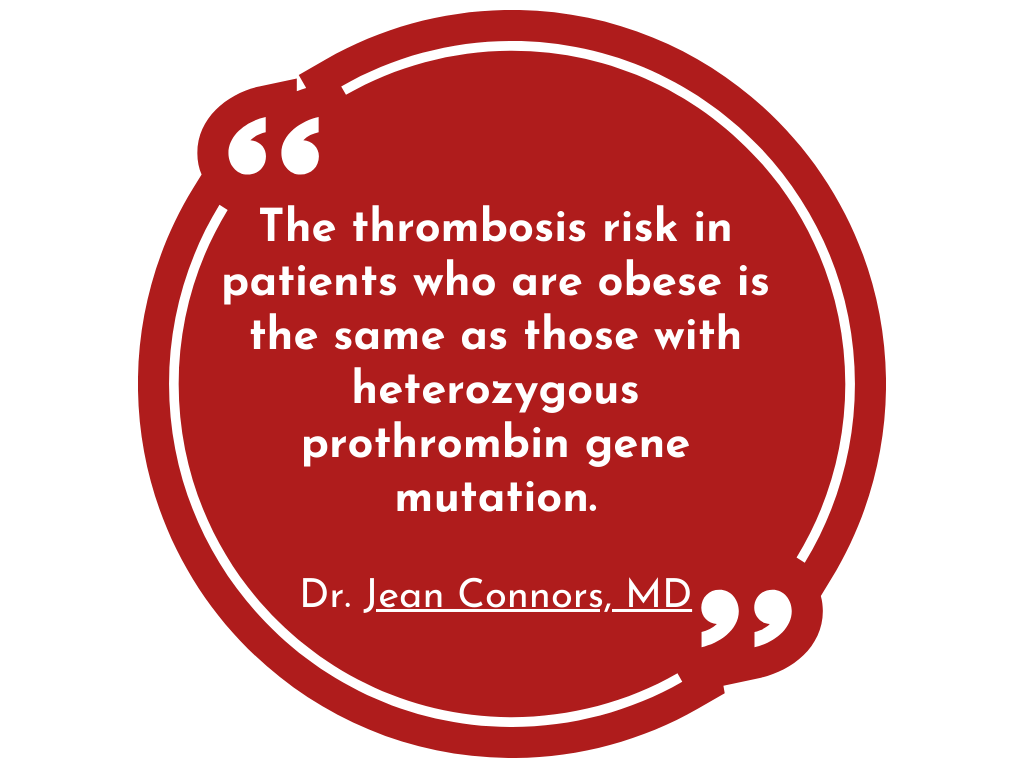
That knowledge gap is greater for women with a history of blood clots, especially when hormone therapy (HT)(MT) comes into play.
In healthy women with a negative risk history, the probability of venous thromboembolism is generally low. This risk increases with age and the presence of additional risk factors, including the presence of cardiovascular disease, obesity, fracture, renal disease, and both congenital and acquired thrombophilic disorders. These risk factors are not rare. Therefore, it is prudent for the prescriber to carefully assess the personal and family history of patients before prescribing HT or ET.
ACOG Committee Opinion
Navigating Menopause and hormone therapy as a blood clot survivor
Women like me with contraindications for hormone therapy are often dismissed from the menopause conversation.
Worse, we’re told we’re doomed to a life of brittle bones, dusty veins and a host of cardiovascular and other health issues if we don’t “replace” our hormones.
Despite current major medical society guidelines that do not recommend hormone therapy for primary prevention of cardiovascular disease, dementia, and osteoporosis.
Labeled as “uneducated” on the latest research if we question the safety of hormone therapy as it specifically relates to us.
Health decisions should never be made out of fear or emotions.
They need to be made from evidence-based education with context and nuance.
Empowering women to make the safest and most effective menopause decisions for their individual health and risk factors.
When it comes to making hormone therapy decisions, (any health decision, really) women should understand there is a difference between studies using healthy women vs women with a history of blood clots.
There’s also a difference between women with a provoked blood clot vs an unprovoked blood clot.
small differences that oftentimes changing the risk vs benefit conversation.
These differences require a healthcare professional who practices from a place of context vs slapping a generalized study on all women.
Val Conley, Founder Speaking of Blood Clots
Life after blood clots is all about risk vs benefit
Here’s why it gets a little complicated for women with a history of blood clots making menopause decisions.
The evidence based clinical studies often cited, exclude women with a history of DVT, PE and VTE.
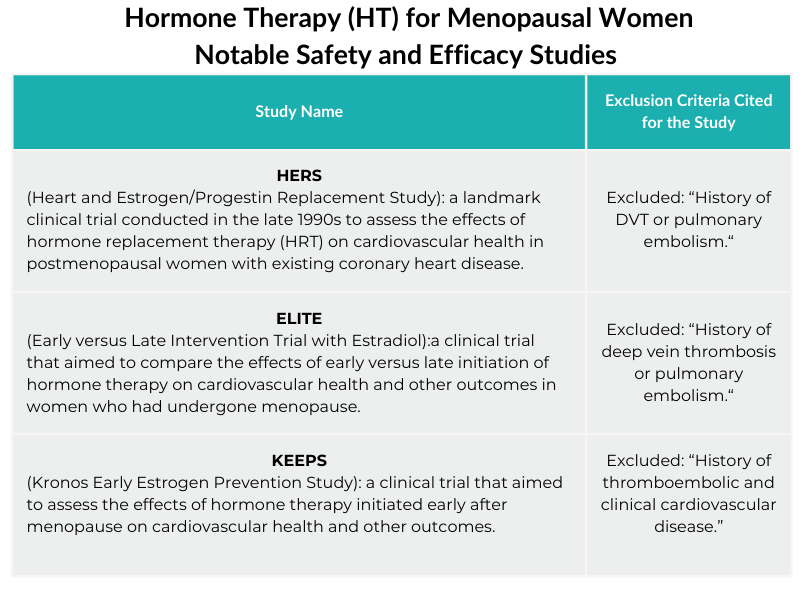 In the menopause conversations there is a tendency to say : “Data (research) Shows.”
In the menopause conversations there is a tendency to say : “Data (research) Shows.”
But “data shows” doesn’t mean the results are safe and effective for all women.
Clinical research often measures the safety and efficacy of drugs and medical procedures for the broadest group of people or situations.
In the case of menopause research, healthy women.
Women who have had a blood clot are not longer healthy women.
We are healthy women with a history.
A history that requires more thought and vigilance from health care providers.
Menopause Education is Different for Women with a History of Blood Clots
No matter your choice, the goal is to educate you so you can become a critical thinker, asking good questions to make an informed decision with the guidance of your care team.
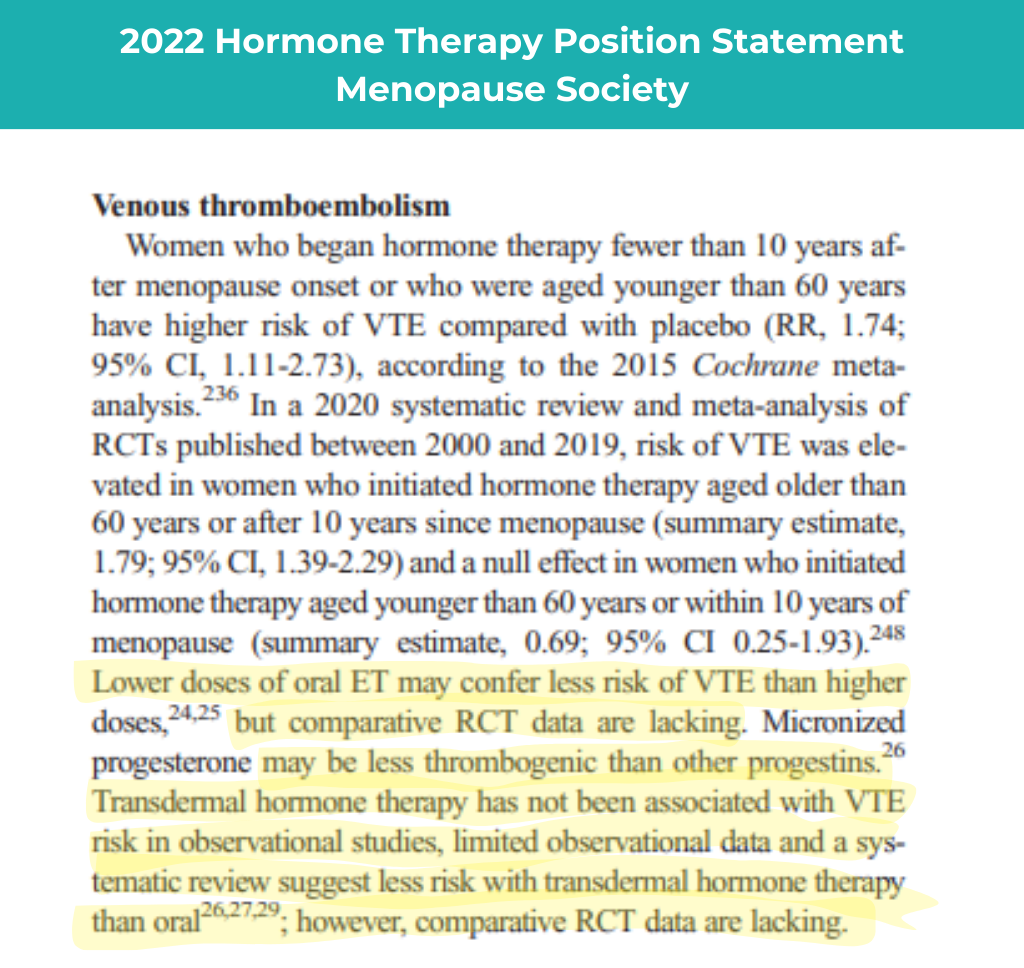
As noted by the Menopause Society when it comes to hormone therapy and venous thromboelism, certain types and routes of hormone therapy MAY be associated with less risk but randomized clinical trials (considered the gold standard or research) are lacking.
Because women with a history of blood clots are an excluded subgroup , context matters in the menopause conversation.
It’s why we teach women to verify the information, paying close attention to language.
Saying “transdermal hormone therapy is fine” based on observational studies to a woman who has survived a blood clot is inaccurate.
“May suggest less risk” in healthy women but the current science is unclear for women with with a history of blood clots is a response more doctors become comfortable saying.
Anything less than that robs women of vigilance to that could save their lives.
It’s the reason physicians advise women with a history of blood clots to avoid hormonal therapy.
It’s not because they’re all “unqualified doctors with outdated opinions.”
In the absence of those clinical trials it’s a best guess by your care team.
How to Start NavigaTING The Menopause Conversation as a blood clot survivor
Having a history of blood clots does not automatically disqualify you from hormone therapy.
It does mean you should seek nuanced conversations with any care provider (even online) based on your clotting history.
It should include an individualized risk assessment including lifestyle habits and baseline cardiovascular health numbers – cholesterol, blood pressure and glucose levels.
A DEXA bone density scan is another baseline measurement to discuss.
Most insurance will cover it at age 65, but having that knowledge earlier (even if it’s paid out of pocket) gives you a better prevention plan heading into menopause.
Whether you choose hormonal or non hormonal options, always know those numbers so you can use them to measure progress and changes and always lead with lifestyle as the foundation for aging well.
Menopause Specific Advise for Blood Clot Survivors
Hormonal Options:
Use the Menopause Society Hormone Guidelines to develop a plan with your hematologist and discuss the following:
- Discuss all the options from least invasive to most.
- Consider a route, dosing and timing recommendation associated with the least amount of risk for blood clots.
- Know and be vigilant for the signs and symptoms of a blood clot. (DVT, PE or VTE)
- Discuss the use of an anticoagulant (blood thinner) as an added layer of protection based on your risks.
- Follow-up. Don’t have a set-it and forget it mentality when it comes to hormone therapy. Have a plan to revisit the effectiveness of HT(MHT) on your symptoms and adjust accordingly.
In healthy women with no background medical problems, transdermal hormone replacement is not associated with an increased risk of thrombosis. However, much less is known about the safety of various HRT preparations in women with a high background risk of thrombosis.
PMID: 36573625
If you choose to manage menopause symptoms without hormone therapy, work with your care team to use the Menopause Society Non-Hormonal Guidelines to develop a plan that includes the following:
Non-hormonal Options:
- Heavy emphasis on positive lifestyle habits. Some research like the WAVS study suggests that certain aspects of a plant-based diet decreases frequency and severity of menopausal hot flashes.
- Discuss the use of non-hormonal medications, stress management tools and other lifestyle habits to manage menopause symptoms.
- Follow-up. If you are still struggling with menopause symptoms that are impacting your quality of life and overall health, speak up. It’s always okay to adjust your health plans to make them work for YOU.

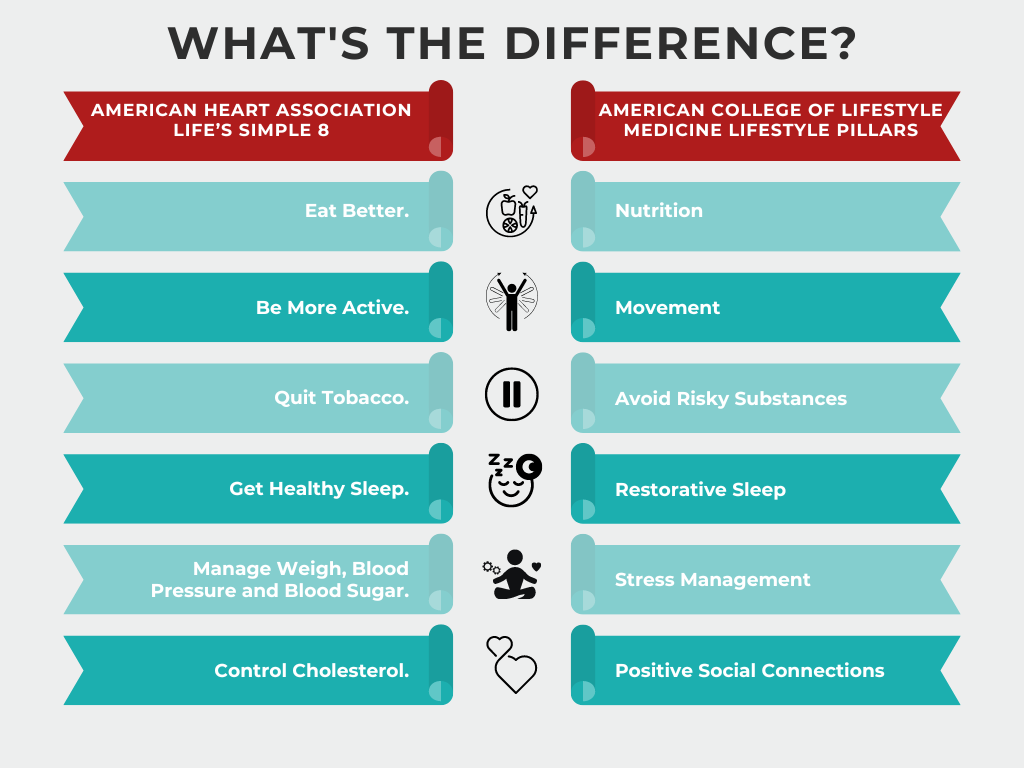

 ARIC revealed among people at low or high genetic risk for VTE, healthier lifestyle factors, particularly normal weight, were associated with a lower incidence of VTE.
ARIC revealed among people at low or high genetic risk for VTE, healthier lifestyle factors, particularly normal weight, were associated with a lower incidence of VTE.